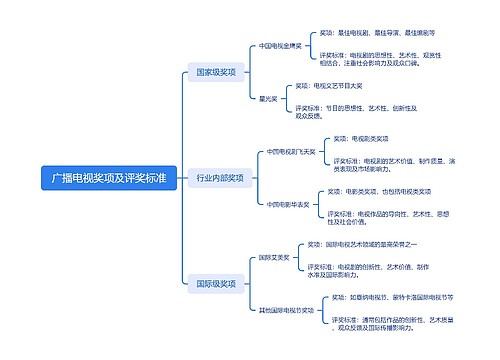
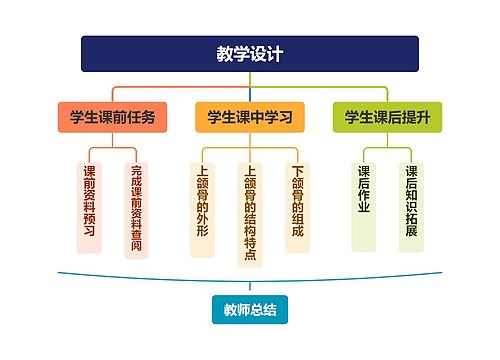
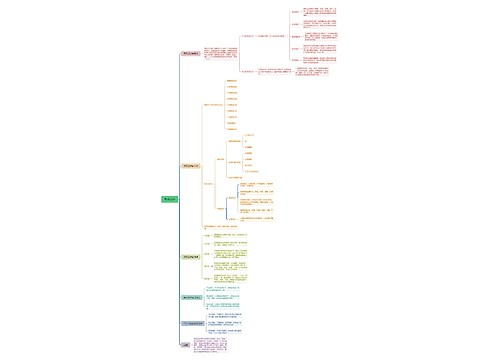
<a id="目录(医脉通临床指南整理)"></a>∙标准与讨论∙思维导图
U952991744
2023-12-12

二线治疗
急性
疗效评估标准
医脉通临床指南整理
树图思维导图提供《<a id="目录(医脉通临床指南整理)"></a>∙标准与讨论∙》在线思维导图免费制作,点击“编辑”按钮,可对《<a id="目录(医脉通临床指南整理)"></a>∙标准与讨论∙》进行在线思维导图编辑,本思维导图属于思维导图模板主题,文件编号是:9f0d8594f80f55620b87d43d0488fed2
思维导图大纲
相关思维导图模版
<a id="目录(医脉通临床指南整理)"></a>∙标准与讨论∙思维导图模板大纲
——急性移植物抗宿主病(2020 年版)
中华医学会血液学分会干细胞应用学组
通信作者:黄晓军,北京大学人民医院,北京大学血液病研究所,国家血液系统疾病临床医学研究中心,造血干细胞移植治疗血液病北京市重点实验室,北京 100044,Email:
基金项目:国家自然科学基金创新群体(81621001)
DOI: 10.3760/cma.j.issn.0253-2727.2020.07.001
Chinese consensus of allogeneic hematopoietic stem cell transplantation for hematological disease
Ⅲ
acute graft-versus-host disease
2020
Stem Cell Application Group, Chinese Society of Hematology, Chinese Medical Association
Corresponding author: Huang Xiaojun, Peking University People
a
mailto:wudepei@suda.edu.cnem,wudepei@suda.edu.cn
s Hospital, Peking University, Institute of Hematology, National Clinical Research Center for Blood Diseases, Beijing 100044, China. Email: huangxiaojun@bjmu.edu.cn; Wu Depei, the First Affiliated
Hospital of Soochow University, National Clinical Research Center for Blood Diseases, Jiangsu Institute of Hematology, Suzhou 215006, China. Email:
异基因造血干细胞移植(allo-HSCT)是治疗多种血液系统疾病的有效方法,单倍型造血干细胞移植(haplo-HSCT)的成功使我国造血干细胞移植病例数量快速增长[1-3]。据中国造血干细胞移植登记组报告,2019 年我国 140 家单位实施allo-HSCT 近万例,其中haplo-HSCT 占60%。尽管allo-HSCT 的疗效不断改善,移植物抗宿主病(GVHD)仍然是主要的合并症和死亡原因。目前急性GVHD 的国际指南中的证据多来自HLA 相合同胞供者(简称同胞相合)移植和非血缘供者移植,各种指南的推荐存在差异,推荐的疗效评判标准和严重程度分度标准也不尽相同[4- 5]。与国外allo-HSCT 以HLA 相合移植和非血缘供者移植为主的模式明显不同,我国haplo-HSCT 占第一位。鉴于我国的移植现状,加之各移植单位规模差别较大,急性GVHD 的处理经验难免存在差别,所以有必要制定中国的专家共识。本共识在国际指南基础上纳入了中国医师在该领域的主要研究成果和临床经验,旨在形成适合中国情况的诊疗规范,为各移植单位提供指导性意见,
并为移植中心之间的交流和合作奠定良好基础。共识由22 位本领域的权威专家参与讨论制定。
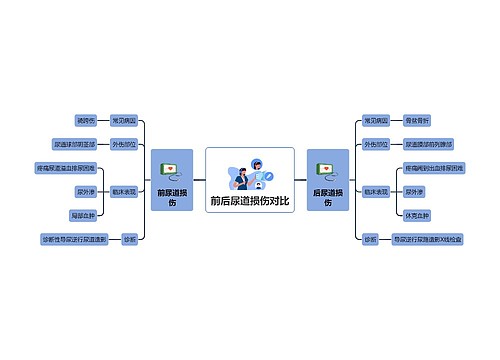
一、急性GVHD 的定义和发生率
(一)急性GVHD 的定义
GVHD 指由异基因供者细胞与受者组织发生反应导致的临床综合征。美国国立卫生研究院
(NIH)的定义将急性 GVHD 分为经典急性GVHD 和晚发急性GVHD:经典急性 GVHD 一般指发生在移植后100 d(+100 d)以内,且主要表现为皮肤、胃肠道和肝脏三个器官的炎性反应;晚发急性GVHD 指具备经典急性GVHD 的临床表现、但发生于+100 d 后的GVHD。晚发急性GVHD 包括以下几种情况:+100 d 后新发生的急性GVHD、已获控制的经典急性GVHD 在+100 d 后再激活、经典急性GVHD 延续至+100 d 后。当急性GVHD 表现和慢性GVHD 同时存在时,诊断为重叠慢性GVHD。供者淋巴细胞输注(DLI)后急性GVHD 诊断以DLI 时间为计时起点,其他与移植后急性GVHD 诊断标准相同[5-7]。
<a id="二、急性GVHD的危险因素"></a><a id="三、急性GVHD的药物预防"></a>(二)急性GVHD 的发生率
国内资料显示,中度和重度急性GVHD 发生率为13%~47%,发生率的差异主要与危险因素不同有关[8-25]。在同胞全相合移植中,Ⅱ~Ⅳ、Ⅲ/Ⅳ度急性GVHD发生率分别为13%~35%、5.0%~7.7%[8-13];在非血缘供者移植中,Ⅱ~Ⅳ、Ⅲ/Ⅳ度急性GVHD发生率分别为12.5%~47.0%、6.6%~13.5%[14- 16];在haplo-HSCT 中,Ⅱ~Ⅳ、Ⅲ/Ⅳ度急性GVHD 发生率分别为18.5%~43.9%、7.9%~13.8%[17- 22];在脐血移植中,Ⅱ~Ⅳ、Ⅲ/Ⅳ度急性GVHD 发生率分别为 28.0%~30.6%、15.0%~19.4%[23- 24]。在接受同胞全相合移植的再生障碍性贫血患者中,重度急性GVHD 发生率最低。
二、急性GVHD 的危险因素
在中国,haplo-HSCT 主要采用基于粒细胞集落刺激因子(G-CSF)和抗胸腺细胞球蛋白(ATG)的非体外去T 细胞移植模式(北京方案)。haplo-HSCT 中急性GVHD 的危险因素与同胞全相合移植和非血缘供者移植中的危险因素并不完全相同,而且通过改进急性GVHD 的预防方案不同程度地削弱了这些危险因素的作用[2,12,25]。
(一)移植类型
既往认为急性GVHD 与HLA 不合的程度有关。近二十年来,大量资料表明,在同胞全相合移植、非血缘供者移植和 haplo-HSCT 三种移植类型中,重度急性GVHD 发生率并无明显差别[8-9,11]。早期报告haplo-HSCT 的Ⅱ~Ⅳ度急性GVHD 发生率高于同胞全相合移植,经优化供者选择及基于危险度的GVHD 分层预防,Ⅱ~Ⅳ度急性 GVHD 发生率在haplo-HSCT 和非血缘供者移植中呈降低趋势[2,12,18-19]。
(二)供受者HLA 不相合的位点数量
在非血缘供者移植中,急性GVHD 发生率随着HLA 不相合位点数量增加而增高[9,14- 16]。在 haplo- HSCT 中,Ⅱ~Ⅳ度急性GVHD 和HLA 不相合位点数量无关[2, 17, 20]。
(三)性别与年龄
在同胞全相合移植中,供者为女性(尤其是多次妊娠者)的患者具有较高的急性GVHD 发生率, 男性受者与女性供者、老年受者与老年供者均为GVHD 的危险因素[12, 25]。而在haplo-HSCT 中,母亲或非遗传性父体抗原(NIPA)不合同胞供者为急性GVHD 的危险因素[2]。
(四)急性GVHD 预防方案
急性GVHD 预防方案与急性GVHD 的发生密切相关,针对高危患者进行急性GVHD 预防方案的改进可减弱危险因素的作用,如在环孢素A(CsA)+ 短程甲氨蝶呤(MTX)方案基础上增加霉酚酸酯
(MMF)和(或)ATG 等能够降低急性GVHD 的发生率、减轻严重程度[10,22]。在母系或旁系供者 haplo- HSCT 中,移植后加入低剂量环磷酰胺可有效降低急性GVHD 的发生率[19]。
三、急性GVHD 的药物预防
药物能有效预防急性GVHD。
(一)同胞相合移植
CsA 联合短程MTX[4- 5]:① CsA:起始剂量
1.5 mg/kg 每12 h 1 次,静脉输注,-1 d 开始(也有主张-7 d 或-9 d 开始),有效谷浓度150~250 μg/L,消化道症状消失后改为口服。一般情况下恶性疾病移植后3 个月CsA 渐减,+6 个月停用,但应根据复发风险和GVHD 情况酌情缩短或延长CsA 应用时间;良性疾病(如重型再生障碍性贫血)移植后1 年CsA 减停,根据嵌合体和GVHD 情况酌情缩短或延长CsA 应用时间。当CsA 不耐受时可更换为他克莫司,初始剂量 0.02~0.03 mg·kg-1 ·d-1 持续输注,一般有效血浓度为 7~12 μg/L,消化道症状消失后改为口服给药,减量原则同 CsA。②MTX:+1 d 15 mg/m2,+3 d、+6 d 10 mg/m2,静脉输注给药。回顾性研究结果提示在同胞全相合移植中+11 d 是否应用MTX 对急性GVHD 没有影响[4,26]。每次MTX 用药结束24 h 后采用甲酰四氢叶酸钙解救。
MMF 及其他:在上述基础预防方案基础上加用MMF 或低剂量兔抗人胸腺细胞球蛋白(rATG) 可进一步减低GVHD 发生率[10,22]。MMF 用法:成人或体重>35 kg儿童1.0 g/d,小儿一般30 mg·kg-1·d-1,分 2~3 次口服。MMF 一般和CsA 同时开始应用
(或+1 d 开始给药),植活或+30 d 停用。
(二)haplo-HSCT 和非血缘供者移植
CsA+短程MTX+MMF+ATG:CsA 用法及用量同上。恶性血液系统疾病移植 100 d 后CsA 渐减,移植后6~9 个月停用(可根据复发风险和急性GVHD 情况进行调整);重型再生障碍性贫血等良性疾病移植后1 年减停CsA。如CsA 不耐受,可改为他克莫司,用法同上。
MTX 用法同上,在重度口腔黏膜炎时+ 11 d MTX 可不用。
MMF 用量和开始时间同上,在非血缘供者移植和haplo-HSCT,通常在植入后减半,移植后2~3个
<a id="四、急性GVHD 的鉴别诊断和严重程度分度标准"></a>月停药(可根据复发风险、GVHD 和是否合并感染等情况进行调整),在无GVHD 的高复发风险或病毒感染患者中酌情缩短MMF 疗程。
ATG 在国内最多应用的是rATG,推荐总剂量 7.5~10 mg/kg,-5~-2 d 分次输注[17-21]。
其他:近年针对 GVHD 高危患者开展一些探索,如在haplo-HSCT 中以生物标志(骨髓移植物的CD4+细胞/CD8+细胞比值)为指导分层短期应用低剂量糖皮质激素、在母系或旁系 haplo-HSCT 后加用低剂量环磷酰胺,均能有效降低急性 GVHD 发生率[18-19]。
(三)脐血干细胞移植
CsA 联合MMF:CsA 和MMF 用法与同胞全相合移植相同。CsA 也可采用持续静脉滴注方式给药,平均血药浓度200~300 μg/L。如恶性血液病无GVHD 迹象,一般移植后2 个月CsA 开始逐渐减量, 至少用至移植后6 个月。
关于ATG 的应用:既往脐血干细胞移植多用ATG,近年来有学者认为不用ATG 也是可行的。孙自敏等[24 ]采用清髓性预处理方案联合CsA+MMF 预防GVHD 进行非血缘脐血干细胞移植,对照组为清髓性预处理方案联合CsA+MMF+MTX 或ATG- FreseniusS(7.5 mg·kg-1·d-1×3 d)预防GVHD 进行的非血缘脐血干细胞移植,两组间Ⅱ~Ⅳ、Ⅲ/Ⅳ度急性GVHD 的发生率差异均无统计学意义,而不含ATG 组的植入率、无病生存率和总生存率明显优于使用ATG 组,差异有统计学意义。
(四)DLI[27-28]
DLI 一般输注G-CSF 动员的淋巴细胞,也可以输注直接采集的供者淋巴细胞,其主要风险是GVHD 发生率和致死率增高,不同类型 DLI 的GVHD 预防方案有所不同。
预防性DLI:一般情况下,在给予预防性DLI时CsA 尚在应用中,DLI 时将CsA 调整至有效浓度。DLI 后CsA 的应用时间因移植类型(同胞全相合移植或haplo-HSCT)、DLI 距移植的时间、输注细胞种类(G-CSF 动员与否)而有所差异。
干预性DLI:CsA 在DLI 前1 d 开始应用并维持有效血药浓度。持续时间依不同移植类型而定, 建议同胞全相合移植患者 DLI 后 4~6 周减停, haplo-HSCT 患者DLI 后 6~8 周减停。干预性DLI 后也可单用MTX 预防GVHD,DLI 后1、4、8 d 各给药1 次,以后10 mg 每周1 次共4~6 次。
治疗性DLI:一般采用 CsA,用法与干预性
DLI 相同。黄晓军等认为治疗性DLI 后短期应用免疫抑制剂可预防重症GVHD 发生,而未影响移植物抗白血病(GVL)效应;在haplo-HSCT 后血液学复发的患者中,DLI 后采用MTX 预防急性GVHD 比用 CsA 可以更好保留GVL 效应。MTX 用法同干预性DLI[29]。也有人认为既往无重症 GVHD 病史的患者,同胞全相合移植的治疗性DLI 后用可MTX 或不用药物预防。
四、急性 GVHD 的鉴别诊断和严重程度分度标准
急性GVHD 的诊断和分度主要依赖皮肤、胃肠道和肝脏的受累情况。
(一)急性GVHD 临床表现[4,30-31]
皮肤:皮肤是急性 GVHD 最多累及的靶器官,表现为斑丘疹,多始于头颈部、耳后、面部和肩部,多累及手掌、足心。患者常无明显不适或仅有轻度瘙痒、疼痛。
胃肠道:胃肠道是急性GVHD 第二位受累的靶器官,上消化道和下消化道均可累及。上消化道急性GVHD 主要表现厌食消瘦、恶心呕吐,下消化道急性GVHD 表现为水样腹泻、腹痛、便血和肠梗阻。下消化道急性GVHD 与移植后非复发相关死亡密切相关。
肝脏:肝脏急性GVHD 表现为胆汁淤积导致的高胆红素血症、伴有或不伴有肝脏酶谱增高[32]。DLI 后急性GVHD 患者仅表现肝脏酶谱增高[33],一般认为属于慢性GVHD,也有学者认为表现更似急性GVHD。
其他表现:随着haplo-HSCT 的广泛开展,除了上述三大器官典型急性GVHD 表现之外,临床医师观察到疑似免疫原因导致发热和肺、中枢神经系统损伤的现象,有学者认为可能是急性GVHD 的特殊表现,因为临床上鉴别诊断非常困难,这些表现是否归于急性GVHD 尚有待进一步研究。
(二)诊断及鉴别
急性GVHD 主要为临床诊断,需要注意排除其他可能情况,尤其在急性GVHD 表现不典型或治疗效果欠佳时,鉴别诊断尤为重要[4-5]。
皮肤急性GVHD 需要与导致皮疹发生的其他情况(预处理毒性、药疹或感染性皮疹等)进行鉴别;重度急性GVHD 可以扩展至全身,表现为大疱甚至表皮剥脱,与Stevens-Johnson 综合征或中毒性表皮坏死松解症进行鉴别。鉴别困难时可以考虑皮肤活检[4-5]。
当患者食欲不振、恶心和呕吐时,可能为上消化道急性GVHD,仅表现上消化道症状时需要和念珠菌病、疱疹病毒感染和非特异性胃炎相鉴别[4-5]。上消化道急性GVHD 的诊断:食欲不振伴体重下降、恶心持续至少3 d,或每天至少2 次呕吐持续至
少2 d。确诊需要胃或十二指肠活检病理结果[5-6]。当腹泻为急性GVHD 初始表现时,应注意与引
起腹泻的其他原因相鉴别,包括感染(艰难梭菌、巨细胞病毒、EB 病毒、腺病毒、轮状病毒等)、药物不良反应、预处理毒性、血栓性微血管病、消化性溃疡等。近年有研究将生物标志物ST2、REG3α或Elafin 等4 因子组合应用于胃肠道急性GVHD 的鉴别诊断及预后判断[34-35],在常规应用于临床前尚需进一步
研究。
当诊断肝脏急性GVHD 时需与引起高胆红素血症的其他原因相鉴别,如预处理相关毒性、药物性肝损伤、肝窦阻塞综合征、脓毒症相关胆汁淤积和病毒性肝炎等。肝活检诊断急性GVHD 应在权衡风险和获益后谨慎采用。
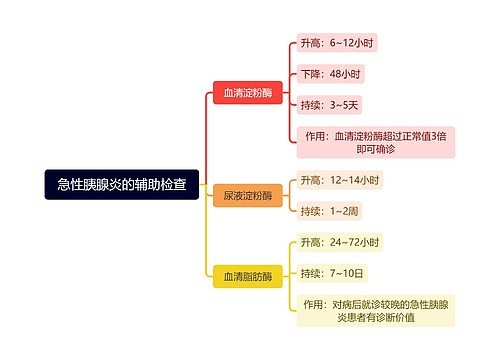
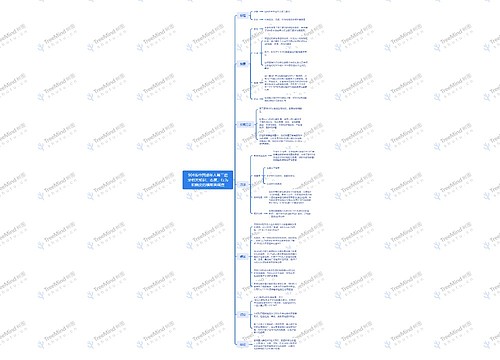
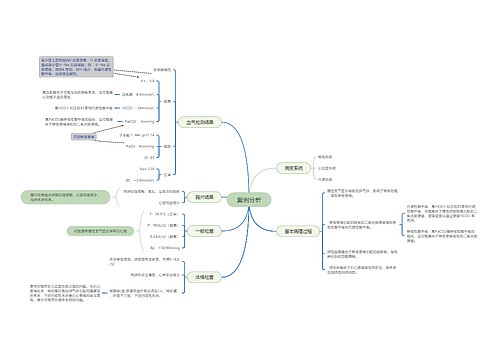
(三)急性GVHD 的分度标准
急性GVHD 的严重程度分度标准是根据急性GVHD 对移植后非复发相关死亡的影响程度制定的,采用皮肤、胃肠道和肝脏急性GVHD 分别积分后再形成总的分度。主要有三种分度标准,其中临床最常采用改良Glucksberg 标准(表 1),近年来急性GVHD 国际联盟(MAGIC)分级标准应用有增多
表
累及器官
项目
皮肤
肝脏-胆红素血症
胃肠道
分级
1 级
皮疹面积<25%a
总胆红素2~3 mg/dlb
腹泻量>500 ml/dc 或持续性恶心d
2 级
皮疹面积25%~50%
总胆红素3.1~6 mg/dl
腹泻量>1 000 ml/d
3 级
皮疹面积>50%,全身红斑
总胆红素6.1~15 mg/dl
腹泻量>1 500 ml/d
4 级
全身红皮病伴大疱形成
总胆红素>15 mg/dl
严重腹痛和(或)肠梗阻
分度e
Ⅰ度
1~2 级
Ⅱ度
Ⅲ度
Ⅳ度f
1~3 级
4 级
1 级
2~3 级
4 级
1 级
2~4 级
注:a 使用9 分法或烧伤图表确定皮疹程度;b 以总胆红素表示范围(如果已经记录了导致总胆红素升高的其他原因,则将其降一级);c 腹泻量适用于成人,儿童(≤14 岁)患者腹泻量应基于体表面积计算(如果记录了腹泻的另一个原因,则将其降一级);d 持续恶心并有胃/十二指肠 GVHD 的组织学证据;e 作为授予该等级所需的最低器官受累程度的分级标准;f Ⅳ度也可能包括较少的器官受累,但功能状态极度下降
表
分级
皮疹(仅活动性红斑)
肝脏
上消化道
下消化道(排便)
0 级
无活动性(红斑)GVHD 皮疹
总胆红素<2 mg/dl
无或间歇性恶心、呕吐或厌食
成人:<500 ml/d或<3 次/d
儿童:<10 ml·kg-1·d-1 或<4 次/d
1 级
<25%
总胆红素2~3 mg/dl
持续性恶心、呕吐或厌食
成人:500~999 ml/d 或3~4 次/d
儿童:10~19.9 ml·kg-1·d-1 或4~6 次/d
2 级
25%~50%
总胆红素3.1~6 mg/dl
成人:1 000~1 500 ml/d 或5~7 次/d儿童:20~30 ml·kg-1·d-1 或7~10 次/d
3 级
>50%
总胆红素6.1~15 mg/dl
成人:>1 500 ml/d 或>7 次/d
儿童:>30 ml·kg-1·d-1 或>10 次/d
4 级
全身红斑(>50%)伴水疱形成或表皮剥脱(>5%)
总胆红素>15 mg/dl
严重腹痛伴或不伴肠梗阻或便血(无论排便量如何)
注:整体临床分级(基于最严重的靶器官受累):0 度:无任何器官1~4 级;Ⅰ度:1~2 级皮肤,无肝脏、上消化道或下消化道受累;Ⅱ度:3 级皮疹和(或)1 级肝脏和(或)1 级上消化道和(或)1 级下消化道;Ⅲ度:2~3 级肝脏和(或)2~3 级下消化道,0-3 级皮肤和(或)0~1 级上消化道;
Ⅳ度:4 级皮肤、肝脏或下消化道受累,0~1 级上消化道受累。儿童:≤14 岁
<a id="五、疗效评估标准及糖皮质激素耐药急性GVHD的定义"></a>趋势(表2)[6,36],此外还有IBMTR 分级系统[37-38]。
五、疗效评估标准及糖皮质激素耐药急性
GVHD 的定义
急性GVHD 开始治疗后每天评估疗效,及时识别糖皮质激素无效的患者。
(一)疗效评估标准
疗效评估通过各个靶器官的急性GVHD 分级和整体分度与初始急性GVHD 情况的比较获得。完全缓解(CR)指所有受累器官的急性GVHD 表现完全消失;部分缓解(PR)指所有初始受累器官的急性GVHD 改善(至少降低一个级别)但未达到CR,无其他任何靶器官急性 GVHD 恶化;无反应
(NR)指任何器官的急性GVHD 严重程度无改善也<a id="六、急性GVHD的治疗"></a>没有恶化或患者死亡;进展(PD)指至少 1 个靶器官的急性GVHD 加重(至少增加1 个级别),伴或不伴其他器官急性GVHD 的改善。PD 和NR 为治疗无效[4-6,38]。
(二)糖皮质激素耐药急性GVHD 的定义
《 Thomas' Hematopoietic Cell Transplantation: Stem Cell Transplantation》(第5 版)将一线治疗 3 d 评估为PD、7 d 评估为NR 或14 d 未达CR 的情况定义为糖皮质激素耐药[30]。在2018 年欧洲骨髓移植学会- NIH- 国际骨髓移植研究中心(EBMT- NIH- CIBMTR)的标准命名中,急性GVHD 疗效评估时, 将一线糖皮质激素开始治疗后3~5 d 内疗效评估为PD 或治疗5~7 d 内疗效评估为NR 或包括糖皮质激素在内的免疫抑制剂治疗28 d 未达CR 定义为糖皮质激素耐药。此外,将一线治疗糖皮质激素不能减量或减量过程中急性GVHD 再激活定义为糖皮质激素依赖。糖皮质激素耐药和糖皮质激素依赖统称为糖皮质激素治疗失败[5-6]。
六、急性GVHD 的治疗
原则上Ⅰ度急性GVHD 可以密切观察和局部治疗,Ⅱ度及以上急性GVHD 诊断后应立即开始一线治疗,但在非血缘供者移植和haplo-HSCT 中早期发生的急性GVHD 往往进展较快,也应立即开始一线治疗。
(一)一线治疗
一线治疗药物为糖皮质激素,最常用甲泼尼龙,推荐起始剂量1 mg·kg-1·d-1 或2 mg·kg-1·d-(1 分 2 次静脉注射),同时将 CsA 谷浓度调整至 150~
250 μg/L 并及时评估糖皮质激素疗效[4,40-41]。
若疗效评估为有效,急性GVHD 达CR 后缓慢减少糖皮质激素用量,成年患者一般每5~7 d 减量
甲泼尼龙10~20 mg/d(或等效剂量其他类型糖皮质激素),4 周减至初始量的10%。儿童患者参照成人按比例缓慢减量。若判断为糖皮质激素耐药,需加用二线药物,并减停糖皮质激素;如判断为糖皮质激素依赖,二线药物起效后减停糖皮质激素。
(二)二线治疗
原则上在维持CsA 有效浓度基础上加用二线药物,并及时评估疗效,当一种二线药物无效后再换用另一种二线药物。国际上尚无统一的二线药物选择流程,一般遵循各自中心的用药原则。鼓励患者参加临床试验。
抗白细胞介素2 受体抗体(IL-2RA)单抗(巴利昔单抗):是迄今国内最多选用的急性GVHD 二线药物。巴利昔单抗对成人糖皮质激素耐药急性GVHD 患者的总有效率达 78.7% ~86.8% ,CR 率达 60.9% ~69.8% ;对儿童 haplo-HSCT 后糖皮质激素耐药急性GVHD 的总有效率达85%,CR 率为 74%[42- 44]。巴利昔单抗推荐用法:成人及体重≥ 35 kg 儿童每次 20 mg 、体 重< 35 kg 儿童每次10 mg,+1、+3、+8 d 各给药1 次,以后每周1 次,使用次数根据病情而定。
MTX:是由中国医师最先用于急性GVHD 治疗的药物。黄晓军团队应用MTX 联合低剂量甲泼尼龙(0.5 mg·kg-1·d-1)一线治疗急性GVHD,总有效率达81%,皮肤、胃肠道和肝脏急性GVHD 的有效率分别为88%、75%、81%[45]。MTX 二线治疗急性 GVHD 也取得很好疗效,治疗急性GVHD 的有效率为94%,治疗DLI 后GVHD 的有效率为100%,对于皮肤、胃肠道、肝脏GVHD 的有效率分别为100%、60%、71%[46]。推荐 MTX 用法:成人每次 10 mg,
+1、+3、+8 d 各给药1 次,以后每周1 次,静脉或口服给药。儿童患者酌减。MTX 的主要不良反应为血液毒性和口腔溃疡,适用于血象良好且没有口腔溃疡的患者。
芦可替尼(Ruxolitinib):刚被美国FDA 批准用于糖皮质激素耐药急性GVHD 的治疗[47-48]。推荐用法:成人初始剂量为10 mg/d(分2 次口服),3 d 后若血液学参数稳定且未发生治疗相关不良反应可调整剂量至20 mg/d。体重≥25 kg 的儿童患者,初始剂量为10 mg/d(分2 次口服);体重<25 kg 的儿童患者,初始剂量为5 mg/d(分2 次口服)。主要不良反应是血液学毒性和增加感染风险(尤其是病毒感染)。芦可替尼国内应用经验有限,相关临床试验正在进行中。
其他:可供选择的二线药物还有非吸收的糖皮 质 激 素 、 霉 酚 酸 (MPA) 类 药 物 、 益 赛 普
(Etanercept)、他 克莫 司(Tacrolimus)、西 罗莫司
<a id="七、受累器官的局部管理和患者的整体管理"></a>(Sirolimus)等[4]。
(三)其他治疗
ATG、间充质干细胞(MSC)、粪菌移植等也有应用。此外,维多珠单抗(Vedolizumab)、托珠单抗
(Tocilizumab)、英夫利昔单抗(Infliximab)、本妥昔单抗(Brentuximab)、抗CCR5 单抗等均有进一步研究的潜力。
七、受累器官的局部管理和患者的整体管理
(一)强化受累器官的管理
皮肤受累的急性GVHD:加强局部护理,保持清洁,局部应用皮肤保护剂,减少渗出。
胃肠道受累的急性GVHD:应重视胃肠道休<a id="八、总结"></a>息、减少或停止经口摄入、部分或全部胃肠外营养补充热量,重视水电酸碱平衡,当不能除外肠道感染时给与经验性抗生素进行肠道除菌,不建议积极使用收敛剂对症处理,以免导致诊断评估的延误。便血患者加强输血支持。
肝脏受累的急性GVHD:慎用影响肝脏的药物,可以应用熊去氧胆酸。
(二)重视患者的整体管理
发生急性GVHD 时,除了皮肤或黏膜屏障功能受损,免疫功能也受抑制,易于发生各种严重感染, 所以治疗急性GVHD 过程中注意感染的监测和预防,如预防疱疹病毒感染、真菌感染,常规监测巨细胞病毒、EB 病毒等。
八、总结
总之,在过去的十年中,尽管急性GVHD 的防治获得了较大进展(尤其是 haplo-HSCT),但急性 GVHD 仍然是allo-HSCT 最常见的合并症和死亡原因之一,规范并优化急性GVHD 防治对提高移植的成功率十分重要,期望未来可以实现预防和治疗GVHD 方案的个体精准化。本共识将根据相关研究进展和临床实践而不断更新。
(执笔:许兰平、张晓辉)
参与共识制定和讨论的专家(以专家所在单位的首字母排序, 同一单位多个专家按照姓氏首字母排序):安徽省立医院(孙自敏); 北京大学第一医院(任汉云);北京大学人民医院、北京大学血液病研究所(黄晓军、许兰平、张晓辉);福建医科大学附属协和医院(胡建达);广西医科大学附属第一医院(赖永榕);河南省肿瘤医院(宋永平);华中科技大学同济医学院附属协和医院(夏凌辉);解放军总医院第一医学中心(刘代红);解放军总医院第五医学中心(胡亮
钉);陆军军医大学附属第二医院(张曦);南方医科大学南方医院
(刘启发);山东大学齐鲁医院(侯明);上海交通大学医学院附属上海儿童医学中心(陈静);上海交通大学医学院附属瑞金医院(胡炯);苏州大学附属第一医院(唐晓文、吴德沛);新疆医科大学附属第一医院(江明);徐州医科大学附属医院(徐开林);浙江大学医学院附属第一医院(黄河);中国医学科学院血液病医院(韩明哲)
参 考 文 献
[1] Xu L, Chen H, Chen J, et al. The consensus on indications, conditioning regimen, and donor selection of allogeneic hematopoietic cell transplantation for hematological diseases in China- recommendations from the Chinese Society of Hematology[J]. J Hematol Oncol, 2018, 11(1):33. DOI: 10.1186/s13045-018-0564-x.
[2] Wang Y, Chang YJ, Xu LP, et al. Who is the best donor for a related HLA haplotype- mismatched transplant? [J]. Blood, 2014, 124(6):843-850. DOI: 10.1182/blood-2014-03-563130.
[3] Xu LP, Wu DP, Han MZ, et al. A review of hematopoietic cell transplantation in China: data and trends during 2008- 2016[J]. Bone Marrow Transplant, 2017, 52(11):1512- 1518. DOI:
10.1038/bmt.2017.59.
[4] Penack O, Marchetti M, Ruutu T, et al. Prophylaxis and manage- ment of graft versus host disease after stem- cell transplantation for haematological malignancies: updated consensus recommen-
dations of the European Society for Blood and Marrow Trans- plantation[J]. Lancet Haematol, 2020, 7(2):e157- 157e167. DOI: 10.1016/S2352-3026(19)30256-X.
[5] Brown P, Inaba H, Annesley C, et al. Pediatric Acute Lympho- blastic Leukemia, Version 2.2020, NCCN Clinical Practice Guidelines in Oncology[J]. J Natl Compr Canc Netw, 2020, 18(1):81-112. DOI: 10.6004/jnccn.2020.0001.
[6] Schoemans HM, Lee SJ, Ferrara JL, et al. EBMT-NIH-CIBMTR Task Force position statement on standardized terminology & guidance for graft- versus- host disease assessment[J]. Bone Marrow Transplant, 2018, 53(11):1401- 1415. DOI: 10.1038/ s41409-018-0204-7.
[7] Jagasia MH, Greinix HT, Arora M, et al. National Institutes of Health Consensus Development Project on Criteria for Clinical Trials in Chronic Graft- versus- Host Disease: I. The 2014 Diagnosis and Staging Working Group report[J]. Biol Blood Marrow Transplant, 2015, 21(3):389- 401.e1. DOI: 10.1016/j. bbmt.2014.12.001.
[8] Han LJ, Wang Y, Fan ZP, et al. Haploidentical transplantation compared with matched sibling and unrelated donor transplanta- tion for adults with standard-risk acute lymphoblastic leukaemia in first complete remission[J]. Br J Haematol, 2017, 179(1): 120-130. DOI: 10.1111/bjh.14854.
[9] Luo Y, Xiao H, Lai X, et al. T-cell-replete haploidentical HSCT with low- dose anti- T- lymphocyte globulin compared with matched sibling HSCT and unrelated HSCT[J]. Blood, 2014, 124(17):2735-2743. DOI: 10.1182/blood-2014-04-571570.
[10] Rubio MT, D'Aveni- Piney M, Labopin M, et al. Impact of in vivo T cell depletion in HLA- identical allogeneic stem cell transplantation for acute myeloid leukemia in first complete remission conditioned with a fludarabine iv- busulfan myeloablative regimen: a report from the EBMT Acute
Leukemia Working Party[J]. J Hematol Oncol, 2017, 10(1):31. DOI: 10.1186/s13045-016-0389-4.
[11] Yu S, Huang F, Wang Y, et al. Haploidentical transplantation might have superior graft- versus- leukemia effect than HLA- matched sibling transplantation for high-risk acute myeloid leu- kemia in first complete remission: a prospective multicentre co- hort study [J]. Leukemia, 2020, 34 (5):1433- 1443. DOI: 10.1038/s41375-019-0686-3.
[12] Wang Y, Wu DP, Liu QF, et al. Donor and recipient age, gender and ABO incompatibility regardless of donor source: validated criteria for donor selection for haematopoietic transplants[J]. Leukemia, 2018, 32(2):492-498. DOI: 10.1038/leu.2017.199.
[13] Xu LP, Jin S, Wang SQ, et al. Upfront haploidentical transplant for acquired severe aplastic anemia: registry- based comparison with matched related transplant[J]. J Hematol Oncol, 2017, 10
(1):25. DOI: 10.1186/s13045-017-0398-y.
[14] Luo Y, Jin M, Tan Y, et al. Antithymocyte globulin improves
GVHD-free and relapse-free survival in unrelated hematopoietic stem cell transplantation[J]. Bone Marrow Transplant, 2019, 54
(10):1668-1675. DOI: 10.1038/s41409-019-0502-8.
[15] Tie R, Zhang T, Yang B, et al. Clinical implications of HLA
locus mismatching in unrelated donor hematopoietic cell transplantation: a meta- analysis[J]. Oncotarget, 2017, 8(16): 27645-27660. DOI: 10.18632/oncotarget.15291.
[16] Yang F, Lu D, Hu Y, et al. Risk Factors for Graft- Versus- Host Disease After Transplantation of Hematopoietic Stem Cells
from Unrelated Donors in the China Marrow Donor Program
[J]. Ann Transplant, 2017, 22: 384- 401. DOI: 10.12659/aot.
902805.
[17] Wang Y, Liu DH, Liu KY, et al. Long-term follow-up of haploi- dentical hematopoietic stem cell transplantation without in vitro T cell depletion for the treatment of leukemia: nine years of ex- perience at a single center[J]. Cancer, 2013, 119(5):978- 985. DOI: 10.1002/cncr.27761.
[18] Chang YJ, Xu LP, Wang Y, et al. Controlled, randomized, open- label trial of risk- stratified corticosteroid prevention of acute graft-versus-host disease after haploidentical transplantation[J]. J Clin Oncol, 2016, 34(16): 1855- 1863. DOI: 10.1200/JCO.
2015.63.8817.
[19] Wang Y, Wu DP, Liu QF, et al. Low-dose post-transplant cyclo- phosphamide and anti-thymocyte globulin as an effective strate- gy for GVHD prevention in haploidentical patients[J]. J Hema- tol Oncol, 2019, 12(1):88. DOI: 10.1186/s13045-019-0781-y.
[20] Yu W, Wang Y, Wu D, et al. Comparison of efficacy between HLA6/6- and HLA3/6- matched haploidentical hematopoietic stem cell transplant in T-cell-replete transplants between parents and children[J]. Sci China Life Sci, 2019, 62(1):104-111. DOI: 10.1007/s11427-017-9302-1.
[21] Lin R, Wang Y, Huang F, et al. Two dose levels of rabbit antithy- mocyte globulin as graft-versus-host disease prophylaxis in hap- loidentical stem cell transplantation: a multicenter randomized study[J]. BMC Med, 2019, 17(1):156. DOI: 10.1186/s12916- 019-1393-7.
[22] Lai YR, Chen YH, Hu DM, et al. Multicenter phase II study of a combination of cyclosporine a, methotrexate and mycophenolate
mofetil for GVHD prophylaxis: results of the Chinese Bone Marrow Transplant Cooperative Group (CBMTCG)[J]. J Hematol Oncol, 2014, 7:59. DOI: 10.1186/s13045-014-0059-3.
[23] 朱江, 汤宝林, 宋闿迪, 等. 非血缘脐血干细胞移植与同胞造血干细胞移植治疗MDS-EB 和AML-MRC 的对比观察[J]. 中华血 液 学 杂 志 , 2019, 40(4):294- 300. DOI: 10.3760/cma.j.
issn.0253-2727.2019.04.006.
[24] Sun Z, Liu H, Luo C, et al. Better outcomes of modified myeloablative conditioning without antithymocyte globulin versus myeloablative conditioning in cord blood transplantation for hematological malignancies: A retrospective(development) and a prospective(validation)study[J]. Int J Cancer, 2018, 143
(3):699-708. DOI: 10.1002/ijc.31339.
[25] Hahn T, McCarthy PL Jr, Zhang MJ, et al. Risk factors for acute
graft- versus- host disease after human leukocyte antigen- identi- cal sibling transplants for adults with leukemia[J]. J Clin Oncol,
2008, 26(35):5728-5734. DOI: 10.1200/JCO.2008.17.6545.
[26] 陈育红, 黄晓军, 许兰平, 等. 异基因造血干细胞移植中甲氨蝶呤3 次与4 次给药的比较[J].北京大学学报(医学版), 2003, 35
(2):215-216. DOI: 10.3321/j.issn:1671-167X.2003.02.030.
[27] Yan C, Xu L, Liu D, et al. Immunosuppression for 6- 8 weeks
after modified donor lymphocyte infusion reduced acute graft- versus- host disease without influencing graft- versus- leukemia
effect in haploidentical transplan[t J]. Chin Med J(Engl), 2014,
127(20):3602-3609.
[28] Wang Y, Chen H, Chen J, et al. The consensus on the monitor-
ing, treatment, and prevention of leukemia relapse after allogene- ic hematopoietic stem cell transplantation in China[J]. Cancer Lett, 2018, 438:63-75. DOI: 10.1016/j.canlet.2018.08.030.
[29] Yan CH, Xu LP, Liu DH, et al. Low- dose methotrexate may preserve a stronger antileukemic effect than that of cyclosporine
after modified donor lymphocyte infusion in unmanipulated haploidentical HSCT[J]. Clin Transplant, 2015, 29(7):594-605. DOI: 10.1111/ctr.12561.
[30] Forman SJ, Negrin RS, Joseph H, et al. Thomas' Hematopoietic Cell Transplantation: Stem Cell Transplantation[M]. 5th Ed. John Wiley & Sons, Ltd. 2015: 1012-1019.
[31] Harris AC, Young R, Devine S, et al. International, Multicenter Standardization of Acute Graft- versus- Host Disease Clinical Data Collection: A Report from the Mount Sinai Acute GVHD International Consortium[J]. Biol Blood Marrow Transplant, 2016, 22(1):4-10. DOI: 10.1016/j.bbmt.2015.09.001.
[32] 莫晓冬, 许兰平, 刘开彦, 等. 肝酶学改变与急性移植物抗宿主病严重程度的相关性研究[J]. 中华血液学杂志, 2009, 30(12): 816-820. DOI: 10.3760/cma.j.issn.0253-2727.2009.12.006.
[33] Akpek G, Boitnott JK, Lee LA, et al. Hepatitic variant of graft- versus- host disease after donor lymphocyte infusion[J]. Blood, 2002, 100(12):3903-3907. DOI: 10.1182/blood-2002-03-0857.
[34] Srinagesh HK, Ferrara J. MAGIC biomarkers of acute graft- versus- host disease: Biology and clinical application[J]. Best Pract Res Clin Haematol, 2019, 32(4):101111. DOI: 10.1016/j.
beha.2019.101111.
[35] Li X, Chen T, Gao Q, et al. A panel of 4 biomarkers for the early diagnosis and therapeutic efficacy of aGVHD[J]. JCI Insight, 2019, 4(16)DOI: 10.1172/jci.insight.130413.
·536· 中华血液学杂志2020 年7 月第41 卷第7 期 Chin J Hematol,July 2020,Vol. 41,No. 7
[36] Przepiorka D, Weisdorf D, Martin P, et al. 1994 Consensus Conference on Acute GVHD Grading [J]. Bone Marrow Transplant, 1995, 15(6):825-828.
[37] MacMillan ML, Robin M, Harris AC, et al. A refined risk score
for acute graft- versus- host disease that predicts response to initial therapy, survival, and transplant- related mortality[J].
Biol Blood Marrow Transplant, 2015, 21(4):761- 767. DOI:
10.1016/j.bbmt.2015.01.001.
[38] Rowlings PA, Przepiorka D, Klein JP, et al. IBMTR Severity Index for grading acute graft- versus- host disease: retrospective comparison with Glucksberg grade[J]. Br J Haematol, 1997, 97
(4):855-864. DOI: 10.1046/j.1365-2141.1997.1112925.x.
[39] Ruutu T, Gratwohl A, de Witte T, et al. Prophylaxis and treat-
ment of GVHD: EBMT- ELN working group recommendations for a standardized practice[J]. Bone Marrow Transplant, 2014,
49(2):168-173. DOI: 10.1038/bmt.2013.107.
[40] Mielcarek M, Furlong T, Storer BE, et al. Effectiveness and
safety of lower dose prednisone for initial treatment of acute graft- versus- host disease: a randomized controlled trial[J].
Haematologica, 2015, 100(6):842-848. DOI: 10.3324/haematol.
2014.118471.
[41] Bacigalupo A, Milone G, Cupri A, et al. Steroid treatment of acute graft- versus- host disease grade I: a randomized trial[J]. Haematologica, 2017, 102 (12):2125- 2133. DOI: 10.3324/ haematol.2017.171157.
[42] Wang JZ, Liu KY, Xu LP, et al. Basiliximab for the treatment of steroid-refractory acute graft-versus-host disease after unmanipu- lated HLA- mismatched/haploidentical hematopoietic stem cell
transplantation[J]. Transplant Proc, 2011, 43(5):1928- 1933. DOI: 10.1016/j.transproceed.2011.03.044.
[43] Tang FF, Cheng YF, Xu LP, et al. Basiliximab as treatment for steroid- refractory acute graft- versus- host disease in pediatric patients after haploidentical hematopoietic stem cell transplantation[J]. Biol Blood Marrow Transplant, 2020, 26(2): 351-357. DOI: 10.1016/j.bbmt.2019.10.031.
[44] Liu SN, Zhang XH, Xu LP, et al. Prognostic factors and long- term follow-up of basiliximab for steroid-refractory acute graft- versus-host disease: Updated experience from a large-scale study
[J]. Am J Hematol, 2020. DOI: 10.1002/ajh.25839.
[45] Wang Y, Xu LP, Liu KY, et al. Low- dose MTX combined with
low-dose methylprednisolone as a first-line therapy for the treat- ment of acute GVHD: safety and feasibility[J]. Bone Marrow
Transplant, 2011, 46(6):892-898. DOI: 10.1038/bmt.2010.197.
[46] 黄晓军, 江倩, 陈欢, 等. 甲氨蝶呤治疗异基因造血干细胞移植后的移植物抗宿主病[J]. 中华医学杂志, 2005, 85(16):1097- 1101. DOI: 10.3760/j:issn:0376-2491.2005.16.006.
[47] Przepiorka D, Luo L, Subramaniam S, et al. FDA approval summary: ruxolitinib for treatment of steroid- refractory acute graft- versus- host disease[J]. Oncologist, 2020, 25(2):e328- 328e334. DOI: 10.1634/theoncologist.2019-0627.
[48] Zeiser R, von Bubnoff N, Butler J, et al. Ruxolitinib for gluco- corticoid-refractory acute graft-versus-host disease[J]. N Engl J Med, 2020, 382 (19):1800- 1810. DOI: 10.1056/NEJ-
Moa1917635.
(收稿日期:2020-05-20)
(本文编辑:徐茂强)
中华医学会血液学分会第十一届委员会委员名单
主 任 委 员
前任主任委员候任主任委员
副主任委员
吴德沛
王建祥胡 豫
肖志坚 刘启发
赵维莅
张晓辉
常 务 委 员(按姓氏笔画为序)
王景文
牛 挺
方美云
付
蓉
刘代红
刘启发
吴德沛
肖志坚 张 曦
张连生
张晓辉
李 娟
李
薇
李建勇
杨林花
陈协群
周剑峰 周道斌
胡 豫
赵维莅
侯 明
侯
健
黄 河
赖永榕
委员兼秘书长
陈苏宁
委
员(按姓氏笔画为序)
王
昭
王少元
王景文
王季石
牛
挺
方美云
付 蓉
朱尊民 江 明
江
倩
刘 利
刘 林
刘 竞
刘
澎
刘代红
刘启发
纪春岩
闫金松
农卫霞
杜 欣
苏雁华
吴德沛
肖志坚
沈建平
邵宗鸿
张 梅
张 曦
张连生
张晓辉
李 剑
李 娟
李 薇
李文倩
李军民
李建勇
李振宇
杨仁池
杨同华
杨林花
陈协群
陈苏宁
陈洁平
邱 林
罗建民
周 凡
周剑峰
周道斌
胡 豫
赵维莅
赵谢兰
侯 明
侯 健
施 均
姜中兴
姚红霞
徐才刚
高素君
黄 河
黄晓军
黄瑞滨
常英军
崔丽娟
韩 悦
韩艳秋
梁爱斌
曾庆曙
赖永榕
蔡 真
魏 辉
潘耀柱
糜坚青
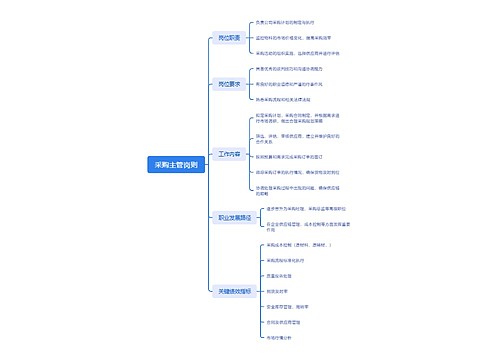
治疗血液系统疾病专家共识(Ⅲ)思维导图模板大纲
查看更多
相似思维导图模版
首页
我的文件
我的团队
个人中心