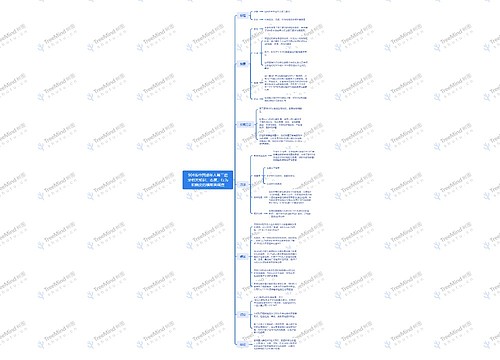
White Lesion思维导图
U767799432
2024-05-29

热烧伤
扁平苔藓
几天到几周内治愈
白色病变英文详述
树图思维导图提供《White Lesion》在线思维导图免费制作,点击“编辑”按钮,可对《White Lesion》进行在线思维导图编辑,本思维导图属于思维导图模板主题,文件编号是:f29b3e6a3396048205458448995b0b70
思维导图大纲
相关思维导图模版
White Lesion思维导图模板大纲
Leukoedema
Uniform opacification of buccal mucosal bilaterally
Unknown cause; more common in smoker
Disappear when mucosa stretched
No Tx needed
-Increased thickness of epithelium-intercellular edema of spinous layer
-Vacuolated cells large and have pyknotic nuclei
White Sponge nevus (Cannon Disease)
Asymptomatic, symmetrical, thickened, white, corrugated or velvety, diffuse plaques affect the buccal mucosa in most instances;
Heraditary; AD; Mutations in either Keratin 4 and/or 13 genes
Appear at birth or early childhood; No Tx needed
Asymptomatic, thick, whitecorrugated plaque; Bilaterally on buccal mucosa
-hyperkeratosis
-Acanthosis
-Clearing of cytoplasm in spinou cell layer
-Perinuclear eosinophilic condensation
Hereditary Benign intraepithelial dyskeratosis (Witkop-Sallmann Syndrome)
Asymptomatic, diffuse, shaggy white lesions of buccal mucosa; EYE lesions - white plaques surrounded by inflamed conjuctiva
Hereditary; AD; Duplication of chromosome 4q35
Primary affect descendants of triracial isolate of people who in North Carolina; appear childhood
Ocular lesion early in life; thick opaque gelatinous plaques; affect bulbar conjunctiva
when lesion active, experience tearing, itching and photophobia
syptomatic ocular lesion should referred to ophthalmologist
Oral lesions like those of white sponge nevus
No Tx on oral lesion
Frictional hyperkeratosis
Asymptomatic, diffuse, white plaque; edentulous ridge, buccal mucosa and tongue; poorly defined borders; not rub off
Chronic irritation
May regress if cause is eliminated
Cheek Chewing
Lip Chewing
Tongue Chewing
Linea Alba (frictional Keratosis); A white line seen on buccal mucosa due to friction of teeth with buccal mucosa
Smokeless Tobacco Keratosis (Snuff Dipper's Lesion)
Asymptomatic white or grey, soft and velvety plaque involving mucosa in direct contact with the snuff or chewing tobacco; indistinct border; usually found in labial and buccal vestibule; flaccid mucosa
Chronic irritation from snuff
or chewing tobacco
Takes 1-5 years to develop; completely reversible; Increased risk of development of Verrucous Ca and SCCa after many years
Soft, fissured, grey-white plaque; poorly defined; induration, ulceration, and pain are not present
-Severity of defect correlated with the quantity and duration of smokeless tobacco use
-Biopsy indicated for lesions with atypical findings
-Habit cessation leads to normal mucosal appearance (usually within 2 weeks) in 98% of cases
-For patients unable to cease the habit, switching to a different tobacco-chewing site is recommended
Lesions that remain after two weeks of cessation should be biopsied!!!
Nicotine Stomatitis (Smokers Palate)
Palatial mucosa is diffusely grey or white with numerous slightly elevated papules with punctate red centers
Develops in response to heat rather than the chemicals in tobacco smoke
Does not appear to have a
premalignant nature;
completely reversible;
-Palatal Mucosa is diffusely grey or white with numerous slightly elevated papules with punctate red centers
-These papules represent inflamed minor salivary glands and their ductal orifices
-Palatal lesion associated with reverse smoking; well-defined reddening of the palatal mucosa (premalignant)
Actinic cheilitis
Lower lip
Chronic UV light exposure
Common premalignant alteration of the lower lip vermillion; May result in SCCa
-Seldom occurs in patients younger than 45 years
-Lesions develop slowly
-Early clinical finding: atrophy (smooth blotchy pale areas), dryness, and fissures of the lower lip with blurring of the margins between vermillion and
adjacent skin
-As lesions progress, rough scaly areas develop
-Eventually, chronic ulcerations may develop , and may suggest
progression to squamous cell carcinoma
Hairy Tongue
Marked accumulation of keratin on filiform papillae of dorsal tongue; Yellow, brown or black; affects midline, sparing lateral and anterior borders
Uncertain; many affected are heavy smokers
Benign process; may be cosmetically objectable
-Accumulation of keratin on filiform papillae on the dorsal surface of tongue-Many affected people are heavy smokers
-Other possible associations: poor oral hygiene, general debilitation, xerostomia inducing drugs, and history of radiation therapy to head and neck
Geographic Tongue (Erythema Migrans)
Multiple well-demarcates zones of erythema (due to atrophy of filiform papillae), surrounded at least partially by elevated yellow-white line.
Unknown
Completely benign; spontaneous regression after months to years
-Typically seen on the anterior 2/3rd of the dorsal tongue mucosa; rarely on other sites
-Appears quickly in one area, healing within a few days or weeks, and then develops in a very different area
-Usually asymptomatic
-May cause a burning to hot and spicy foods
-Rarely is the burning sensation severe and constant;
-topical corticosteroids (betamethasone) rovides relief
-2/3rd patient have a fissured tongue
Dentifrice associated slough (Oral Mucosal Peeling)
Asymptomatic, slough of flimsy
parakeratotic cells
Mucosal reaction to components in toothpaste (sodium lauryl sulphate)
-Most frequently involved areas: oral vestibule, buccal mucosa and gingiva
-Evolution time is quite variable, from 3 days to 10 years, depending on the exposition to the
causal agent
Mucosal Burns
Painful white fibrin exudate covering superficial ulcer with erythematous ring; common
Chemical (aspirin, phenol), heat, electric burns
Heals in days to weeks
Chemical Burn
-Large ulcer following improper use of
bisphosphonate (Alandronate) & Formalin
Thermal Burns
Electric Burn
-Areas of yellow-white epithelial necrosis and areas of erythema
Oral Hairy Leukoplakia
White mucosal plaque that does not rub off; Most cases on lateral borders of tongue; vary from faint, white vertical streaks to thickened, furrowed areas of leukoplakia with a shaggy surface; infrequently cover dorsal tongue
Epstein-Barr viral infection in patients
with AIDS
May also occur in immunosuppressed patients
Development may indicate:
1. disease progression,
2. lack of compliance to ART, or
3. retroviral drug resistance
Treatment not needed; Systemic anti-retroviral drugs produce resolution
HIV-associated OHL; vertical streaks of
keratin along the lateral border of tongue
Idiopathic Leukoplakia
Asymptomatic white patch; cannot be wiped off; > males
Unknown; may be
related to tobacco or
alcohol use
May recur after excision; 5% are malignant; higher risk of carcinoma if dysplasia present
1. Mild epithelial dysplasia: alterations limited principally to the basal and parabasal layers
2. Moderate epithelial dysplasia: alterations from the basal layer to the midportions of the epithelial layer
3. Severe epithelial dysplasia: alterations from the basal layer to the level above the midpoint of the epithelium
Early, thin and homogenous leukoplakia
Well-defined, thin, white plaque
Homogenous and thick leukoplakia
Well-defined, thick, white plaque
Granular Leukoplakia
Granular Erythroleukoplakia
Verrucous Leukoplakia
Keratotic plaques with rough surface projections
Proliferative Verrucous leukoplakia
Extensive leukoplakia with rough surface projections; the plaques proliferate
Lichen Planus
Middle aged adults;
-Skin lesions: purple, pruritic, polygonal plaques (4Ps)
-Reticular LP: posterior buccal mucosa,
bilaterally; asymptomatic; interlacing white
-Erosive LP: symptomatic; atrophic,
erythematous areas with central
ulcerations of various degrees; periphery of atrophic region bordered by interlacing white lines
-Desquamative gingivitis: atrophy and
ulceration confined to gingiva
Unknown; hyperimmune condition mediated by T-cells
Diagnosis of LP
-Reticular LP: based on clinical findings alone
-Erosive LP: sometimes challenging; Diagnosis confirmed by direct immunofluorescent examination of
paralesional tissue submitted in Michel's solution
-Most lesions show the deposition of a shaggy band of fibrinogen at the basement membrane zone
May regress after many years; treatment may only control disease; the question of malignant potential still not resolved; rare malignant transformation
Relationship to stress and anxiety is controversial; recent studies show a link with hypothyroidism
Cutaneous Lichen Planus
Purple, polygonal papules
Reticular Lichen Planus
Interlacing white lines involving buccal mucosa, bilaterally
Erosive Lichen Planus
Ulcerations, with peripheral radiating white lines
Desquamative gingivitis
When atrophy and ulcerations are confined
to the gingival mucosa
Pseudomembranous Candidiasis (Thrush)
Adherent white plaques that resemble
cottage cheese or curdled milk on the oral surface; can be wiped off; underlying mucosa may appear normal or edematous
Symptoms: burning sensation, and an
unpleasant taste
Opportunistic fungus; initiated by exposure of patient to broad-spectrum antibiotics or use of topical
corticosteroids; immunosuppression
Antifungal medications; Usually disappears in 1-2 weeks after treatment; Some chronic cases require long term therapy
White plaques on an erythematous base; can be wiped off with a wet gauze
Fordyce granules
Multiple, yellow or yellow-white papules; asymptomatic; seen primarily in buccal mucosa and lips; variation of normal (80% of population)
Developmental
Ectopic sebaceous glands (Choristoma) of no significance
Yellow papules; asymptomatic
Lymphoid hyperplasia
Asymptomatic, smooth surfaced papules or elevated-yellow nodule; <0.5 cm in diameter; usually found on tonsillar pillars, posterolateral tongue and floor of mouth; covered by intact epithelium; common
Developmental
No significance; lesions remain indefinitely and are usually diagnostic clinically
Palatal lymphoid hyperplasia: Smooth surfaced pink or yellowish papules
Large tonsils; if significant asymmetry is observed, further investigations may be warranted to rule out possibility of
lymphoma or other malignancy
Lingual Tonsil
Smooth-surfaced papule of the posterior lateral tongue represents an enlarged lymphoid
aggregate
Gingival cyst of the adult
Painless, dome-shaped swelling (<0.5 cm in diameter); bluish or blue-grey
In some instances, it may cause cupping out of the alveolar bone
Developmental
Soft tissue counterpart of lateral periodontal cyst
Simple surgical excision
Tense, fluid-filled
swelling on the facial Gingiva
Thin-walled cyst in the gingival soft tissue
Cyst of the newborn
On gingiva: Bohn nodules
On palate: Epstein pearls
Self-healing; burst spontaneously
Bohn Nodules
Epstein Pearls
Parulis (gum Boil)
Erythematous mass of granulation tissue; intraoral opening of sinus tract;
Dental abscess
Occasionally, the non-vital tooth associated with parulis difficult to determine; insert gutta-percha in and examine radiograph
Erythematous mass of granulation tissue
Gutta percha point revealed the source of infection
Lipoma
Asymptomatic; slow-growing, yellowish, soft, smooth-surfaced nodule; pedunculated or sessile; benign neoplasm of fat; occurs in any area
Unknown
Limited growth potential intraorally; recurrence not expected after removal
Soft, yellow, smooth-surfaced, nodular mass
思维导图模板大纲
查看更多
相似思维导图模版
首页
我的文件
我的团队
个人中心