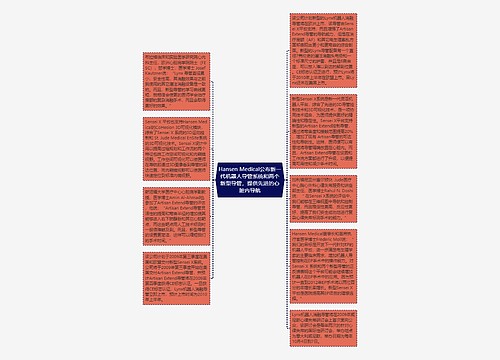
By Laurie Barclay, MDMedscape Medical News
Patients with chronic kidney disease (CKD) on hemodialysis treated with paricalcitol alone had better outcomes than did those treated with both paricalcitol and cinacalcet, according to the results of a multicenter, retrospective study presented at the National Kidney Foundation (NKF) 2008 Spring Clinical Meetings in Dallas, Texas.
"The use of activated vitamin D has been the cornerstone of secondary hyperparathyroidism (SHPT) therapy in CKD patients, and therapeutic decisions regarding the treatment of SHPT have become increasingly complicated with the advent of cinacalcet therapy," presenter and lead author Maria Karalis, MBA, RD, LDN, director of commercial development at Abbott Renal Care in Abbott Park, Illinois, told Medscape Nephrology.
The rationale for paricalcitol treatment in CKD is that vitamin D deficiency and increased calcium levels associated with CKD tend to increase levels of parathyroid hormone (PTH), with development of SHPT as a significant cause of morbidity and mortality. Vascular calcification may result from elevated calcium (Ca) and phosphorus (P) levels.
Paricalcitol, which successfully regulates PTH levels in CKD patients and maintains appropriate Ca and P levels, is one of several vitamin D receptor activators now available to treat patients with SHPT. Calcimimetic agents, such as cincalcet, have also been developed to treat elevated Ca levels as SHPT progresses.
Kamyar Kalantar-Zadeh, MD, PhD, MPH, FAAP, FACP, FASN, FAHA, an associate professor of medicine and pediatrics, and director of off-campus dialysis expansion and epidemiology in the Harbor-UCLA Division of Nephrology and Hypertension at the Los Angeles BioMedical Research Institute, and UCLA David Geffen School of Medicine, was not involved in this study, but provided independent commentary for Medscape Nephrology.
"This historical study indicates that the role of cinacalcet can be an adjunct treatment and that paricalcitol alone can achieve target levels," Dr. Kalantar-Zadeh said.
The iPTH target range of 100 to 300 pg/mL was achieved by 38% of patients treated with Z alone vs 25% of those treated with Z+S. The patients treated with Z alone also fared better than those treated with Z+S in terms of the proportion that reached the Ca target range of 8.4 to 9.5 mg/dL (52% vs 46%) and the P target range of 3.5 to 5.5 mg/dL (48% vs 39%).
"Patients treated with paricalcitol alone had greater achievement of all KDOQI targets than those treated with both paricalcitol and cinacalcet therapy," Dr. Karalis said. "The dose of paricalcitol should be optimized first, based on package insert guidelines, before adding other therapeutic agents."
Based on these findings, the investigators suggest that protocols used to treat SHPT with
cinacalcet before optimizing the dose of vitamin D receptor activator therapy should be reevaluated, especially considering the tremendous pill burden for patients on hemodialysis.
In terms of additional research, Dr. Karalis suggested that time-varying analysis methods may offer additional insights. Dr. Kalantar-Zadeh recommended randomized clinical trials or prospective observational studies.
"The strengths [of this study] include large sample size and inclusiveness of the study population, which minimizes selection bias," Dr. Kalantar-Zadeh concluded. "The limitation is its observational nature, which makes it amenable to confounding by indication, ie, patients who received medication such as cincalcet were those who were probably more resistant to standard treatment."
The study was funded by Abbott Renal Care, and all of the study authors are employed by Abbott.
National Kidney Foundation 2008 Spring Clinical Meetings: Abstract 133. April 2–6, 2008.

 U575789758
U575789758
 U482218638
U482218638