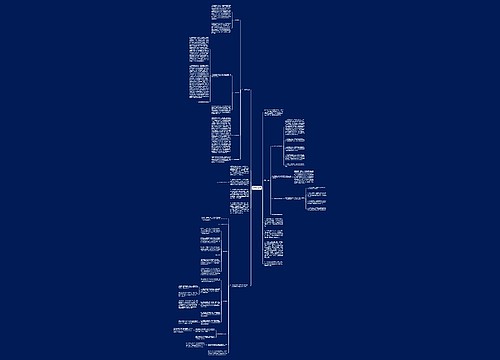
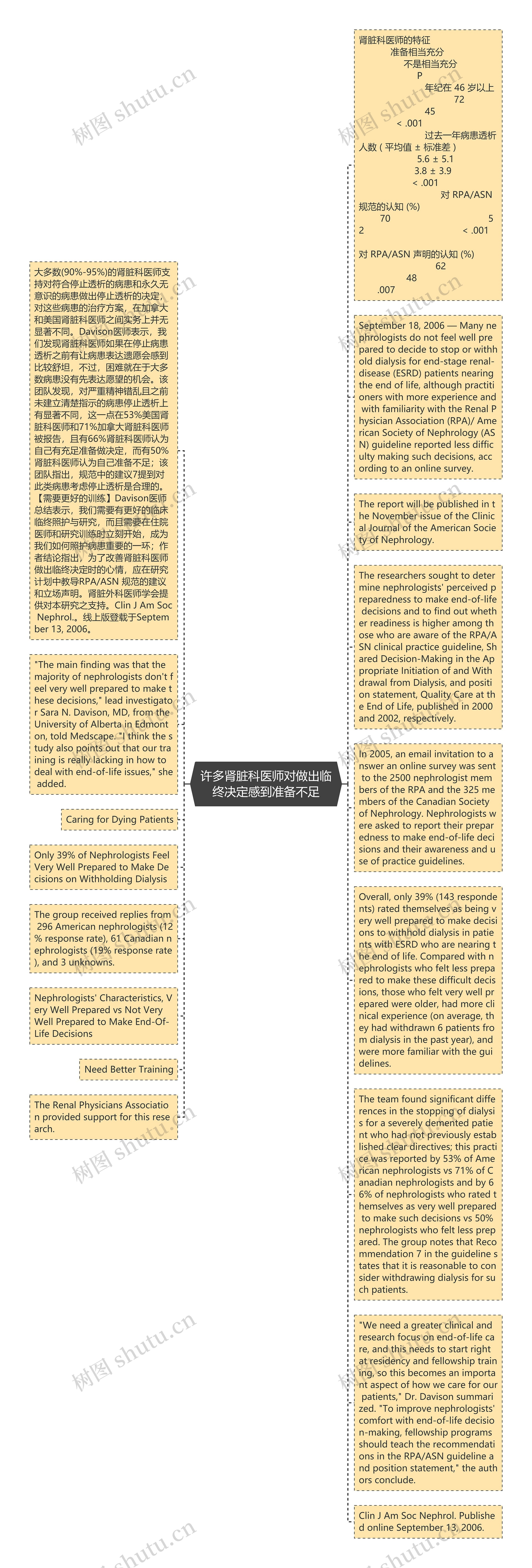
肾脏科医师的特征 准备相当充分 不是相当充分 P 年纪在 46 岁以上 72 45 < .001 过去一年病患透析人数 ( 平均值 ± 标准差 ) 5.6 ± 5.1 3.8 ± 3.9 < .001 对 RPA/ASN 规范的认知 (%) 70 52 < .001 对 RPA/ASN 声明的认知 (%) 62 48 .007
大多数(90%-95%)的肾脏科医师支持对符合停止透析的病患和永久无意识的病患做出停止透析的决定,对这些病患的治疗方案,在加拿大和美国肾脏科医师之间实务上并无显著不同。Davison医师表示,我们发现肾脏科医师如果在停止病患透析之前有让病患表达遗愿会感到比较舒坦,不过,困难就在于大多数病患没有先表达愿望的机会。该团队发现,对严重精神错乱且之前未建立清楚指示的病患停止透析上有显著不同,这一点在53%美国肾脏科医师和71%加拿大肾脏科医师被报告,且有66%肾脏科医师认为自己有充足准备做决定,而有50%肾脏科医师认为自己准备不足;该团队指出,规范中的建议7提到对此类病患考虑停止透析是合理的。【需要更好的训练】Davison医师总结表示,我们需要有更好的临床临终照护与研究,而且需要在住院医师和研究训练时立刻开始,成为我们如何照护病患重要的一环;作者结论指出,为了改善肾脏科医师做出临终决定时的心情,应在研究计划中教导RPA/ASN 规范的建议和立场声明。肾脏外科医师学会提供对本研究之支持。Clin J Am Soc Nephrol.。线上版登载于September 13, 2006。
September 18, 2006 — Many nephrologists do not feel well prepared to decide to stop or withhold dialysis for end-stage renal-disease (ESRD) patients nearing the end of life, although practitioners with more experience and with familiarity with the Renal Physician Association (RPA)/ American Society of Nephrology (ASN) guideline reported less difficulty making such decisions, according to an online survey.
"The main finding was that the majority of nephrologists don't feel very well prepared to make these decisions," lead investigator Sara N. Davison, MD, from the University of Alberta in Edmonton, told Medscape. "I think the study also points out that our training is really lacking in how to deal with end-of-life issues," she added.
The report will be published in the November issue of the Clinical Journal of the American Society of Nephrology.
Caring for Dying Patients
The researchers sought to determine nephrologists' perceived preparedness to make end-of-life decisions and to find out whether readiness is higher among those who are aware of the RPA/ASN clinical practice guideline, Shared Decision-Making in the Appropriate Initiation of and Withdrawal from Dialysis, and position statement, Quality Care at the End of Life, published in 2000 and 2002, respectively.
Only 39% of Nephrologists Feel Very Well Prepared to Make Decisions on Withholding Dialysis
In 2005, an email invitation to answer an online survey was sent to the 2500 nephrologist members of the RPA and the 325 members of the Canadian Society of Nephrology. Nephrologists were asked to report their preparedness to make end-of-life decisions and their awareness and use of practice guidelines.
The group received replies from 296 American nephrologists (12% response rate), 61 Canadian nephrologists (19% response rate), and 3 unknowns.
Overall, only 39% (143 respondents) rated themselves as being very well prepared to make decisions to withhold dialysis in patients with ESRD who are nearing the end of life. Compared with nephrologists who felt less prepared to make these difficult decisions, those who felt very well prepared were older, had more clinical experience (on average, they had withdrawn 6 patients from dialysis in the past year), and were more familiar with the guidelines.
Nephrologists' Characteristics, Very Well Prepared vs Not Very Well Prepared to Make End-Of-Life Decisions
The team found significant differences in the stopping of dialysis for a severely demented patient who had not previously established clear directives; this practice was reported by 53% of American nephrologists vs 71% of Canadian nephrologists and by 66% of nephrologists who rated themselves as very well prepared to make such decisions vs 50% nephrologists who felt less prepared. The group notes that Recommendation 7 in the guideline states that it is reasonable to consider withdrawing dialysis for such patients.
"We need a greater clinical and research focus on end-of-life care, and this needs to start right at residency and fellowship training, so this becomes an important aspect of how we care for our patients," Dr. Davison summarized. "To improve nephrologists' comfort with end-of-life decision-making, fellowship programs should teach the recommendations in the RPA/ASN guideline and position statement," the authors conclude.
The Renal Physicians Association provided support for this research.
Clin J Am Soc Nephrol. Published online September 13, 2006.
 U575789758
U575789758
 U482218638
U482218638